Breast Cancer 101
EVERYTHING YOU NEED TO KNOW ABOUT BREAST CANCER PREVENTION AND RISK REDUCTION:
Breast Cancer 101
How to Reduce Your Risk of Developing Breast Cancer
Are you at High Risk for Developing Breast Cancer?
Breast Cancer Screenings
“ I tested positive for a Cancer-Causing Gene Mutation”
My First Mammogram
THE TIME I WAS ON ELLEN:
October is always a month of mixed emotions for me. We are bombarded to buy everything pink and there is this constant messaging of “Breast Cancer Awareness”. I think we are all aware of Breast Cancer by now. One year I was feeling particularly bitter and asked a young person what their “I heart BOOBIES” bracelet represented, or how it benefited cancer patients. Their reply? “It’s to prevent the awareness of breast cancer.” FACEPLAM.
If you want to support breast cancer patients and research in a more meaningful way, donate directly to trustworthy foundations. Many employers match donations as well, so it’s much more impactful that way.
These bracelets from Oriental Trading provide absolutely ZERO benefit to breast cancer patients or cancer research,
I have been an Oncology Nurse for over a decade and helped thousands of cancer patients over the years and have watched my close relatives walk through cancer treatments. I personally have tested positive for a gene mutation that puts me at higher risk for developing cancer (MUTYH).
Let’s dig in beyond “Awareness” and I’ll share with you ways you can reduce your risk of developing breast cancer and discover it early, which leads to less invasive treatment and better survival rates.
BREAST CANCER 101
There are many variables that contribute to if and how fast a cancer grows. We have control over some of the variables and others, we do not. For example, cancer rates have been rising and a main contributing factor is age. The older we get, the more likely our cells are to make sloppy mistakes while duplicating.
Breast cancer can arise from the ducts (Ductal Carcinoma) or the lobules, which are the milk producing gland (Lobular Carcinoma) or more rarely, the tissue between. There are over 8 different kinds of breast cancer and the most common type is Ductal Carcinoma (70-80% of all breast cancer cases).
Once a suspicious mass is found on imaging, a small tissue sample is taken to see what the cells actually are. A pathologist looks at the cells/tissue under a microscope. They can be anything from completely benign (non-cancerous) to malignant (cancer).
Estrogen is made in our fat tissue all over the body and is produced when menstruating. The most common type of breast cancer is fed by hormones (estrogen and progesterone). Part of a breast cancer diagnosis refers to the hormone receptors, ER, PR and HER2. If the ER (estrogen) and PR (progesterone) receptors are positive, the breast cancer grows when exposed to hormones and those hormones can be blocked as a way to prevent cancer in very high risk patients and help treat cancer. HER2 is a receptor found on the breast cancer cells and if it is positive, then a drug called Herceptin can be used to help kill the cancer cells.
What cancer cells (Lobular Carcinoma) looks like after a breast biopsy, when the pathologist looks at it under a microscope. Photo from Medscape.
Spending money on detoxes and supplements is like buying a decorative wreath for this house. Focus on supporting your body with the foundation of health.
HOW TO REDUCE YOUR RISK OF DEVELOPING CANCER
Detoxes? Clean Beauty?
Supplements? Goji Berries?
BPA free water bottles?
Avoiding Disneyland?
What makes the biggest impact on your health?
THERE ARE A LOT OF BUSINESSES STANDING TO MAKE A LOT OF MONEY FROM SCARING CONSUMERS BY THREATENING CANCER.
5-10% of cancer is caused by cancer-causing genes that are passed down through families (hereditary gene mutations). Spoiler alert, I have one! Read the story of my positive genetic test results below.
What causes that first cell to make an error and turn into a cancer cell?
The vast majority of cancer is cause by OTHER factors. I always highly stress that there are some risks we can control and others we cannot. No one ever deserves cancer and it is never, ever helpful to focus on “why did this person develop cancer”? Below is shared to help YOU reduce your risk for developing cancer.
Knowing your Family History is a great start to learning how to risk reduce, including indications for genetic testing. Photo by Mattie Arts.
YOUR TIME AND ATTENTION ARE PRECIOUS AND IT’S WISEST TO FOCUS ON RISK REDUCTION THAT WE HAVE EVIDENCE FOR, STARTING WITH:
Know your family history. See below to find out when you qualify for genetic testing.*
Make sure you are up to date on cancer screenings (ask your primary care doctor or find one!). In general, cancer screenings start 10 years prior to the youngest family member diagnosed with cancer OR the recommended screening age, whichever is younger.
Get Moving. At least 150 minutes per week of moderate-intensity physical activity; increase to 300 minutes to support weight loss. (World Cancer Research estimates 20% of all cancers in US are related to excess body fat and physical inactivity)
Don’t Smoke. Quit Smoking- it’s not too late!
Limit Alcohol. If you do drink, no more than 1 drink per day for women or 2 for men (3 drinks per week if there is a higher risk of breast cancer).
Risk Reducing medications and surgery can be used for certain high risk populations (such as BRCA 1+ 2 carriers).
Instead of buying supplements, aim to fill 2/3 of your plate with foods high in nutrients and cancer-fighting phytochemicals! If you want to use vitamins, only buy vitamins with 100% of the daily value, not more.
CANCER RISK REDUCING DIET
Eat a mainly plant-based diet packed with phytochemical-rich minimally processed vegetables, fruit, whole grains, beans, legumes, whole soy foods, nuts, seeds, herbs, and spices. Fill 2/3 of your plate and especially dark leafy greens and other richly colored options.
Limit highly processed forms of carbohydrates (i.e: foods made out of flour) and added sugar (limit to no more than 24 grams added sugar/day for women and 36 grams for men).
Avoid red meat and processed meats. If you consume animal foods: choose lean, high quality animal proteins and low fat dairy.
Do not use large doses of vitamin and mineral supplements to prevent cancer; use them instead to help meet basic nutrition needs, or to correct a known nutrient deficiency. There is risk for Nutritional Deficit if there is any dietary restrictions (dairy, carb, animal products) or having symptoms like fatigue or depression (can check iron and vitamin levels). Can use any multivitamin, just check the label for 100% RDV or DV. Don’t use any megadoses of vitamins.
Phytochemicals are more easily absorbed and bioavailable from food than supplements.
Instead of taking probiotics, eat probiotic rich cultured foods and prebiotic fibers that may help promote the growth of good bacteria:
Activia, Yakult, Good Belly, kefir, buttermilk
Kombucha Tea. Raw miso paste
sauerkraut, natto, kimchi, tempeh
Jerusalem artichoke (aka sunchoke)
Asparagus, Banana, Garlic, Leeks, Onions
THANK YOU TO DR MAY CHEN (ONCOLOGIST) , ASTRID SHAPIRO RD AND JULIE SIMCO RD (REGISTERED DIETICIANS), COURTNEY ROWE-TEETER (GENETIC COUNSELOR) AND DR KARAM (GYNECOLOGIC-ONCOLOGIST) FOR CONTRIBUTING.
ARE YOU AT HIGH RISK FOR DEVELOPING BREAST CANCER?
Check to find out if you are at High Risk for Developing Breast cancer by taking the Assessment here.
RISK FOR DEVELOPING BREAST CANCER UNDER 45
If you are under the age of 45, you may have a higher risk for breast cancer if—
You have close relatives who were diagnosed with breast cancer before the age of 45 or ovarian cancer at any age, especially if more than one relative was diagnosed or if a male relative had breast cancer.
You have changes in certain breast cancer genes (BRCA1 and BRCA2), or have close relatives with these changes, but have not been tested yourself.
You have Ashkenazi Jewish heritage.
You received radiation therapy to the breast or chest during childhood or early adulthood.
You have had breast cancer or certain other breast health problems, such as lobular carcinoma in situ (LCIS), ductal carcinoma in situ (DCIS), atypical ductal hyperplasia, or atypical lobular hyperplasia.
You have been told that you have dense breasts on a mammogram.
More information and support for young women who have or are at risk of developing breast cancer can be found at Bring Your Brave.
WHEN TO TALK TO YOUR PRIMARY CARE DOCTOR ABOUT A REFERRAL TO HAVE GENETIC TESTING:
IF YOU HAVE A PERSONAL OR FAMILY HISTORY OF:
Breast, Colon or Endometrial cancer prior to age 50
Ovarian cancer at any age
Male breast cancer at any age
Pancreatic cancer at any age
High Risk, Very High Risk or Metastatic Prostate Cancer at any age
>10-20 cumulative colon polyps (especially adenomas)
Multiple primary cancers in an individual
Multiple affected relatives & generations
Particularly with the same or associated cancer types
Known pathogenic (cancer causing) gene mutation in family
Genetic testing typically starts with the person diagnosed with cancer and if they test positive, then their relatives are tested.
ALL ABOUT MAMMOGRAMS
The purpose of cancer screenings it to catch early cancers, when cure is most likely and treatment is typically less-invasive. Think of “The Squeeze” as a way to help you live longer and see your kids grow up.
WHY IT’S SO IMPORTANT TO STAY ON TOP OF SCREENINGS
“Women participating in the last two breast cancer screening examinations prior to breast cancer diagnosis had the largest reduction in breast cancer death. Missing either one of the last two examinations conferred a significantly higher risk.
The incidence of breast cancers proving fatal within 10 years of diagnosis was 50% lower for serial participants than for serial nonparticipants. Compared to women who attended only one of the two previous screens, women who attended both had 29% fewer breast cancer deaths” (Radiology in ASCO).
Lobular Carcinoma when seen on Mammogram. Image from BiomedCentral.com
“In recent years, a newer type of mammogram called digital breast tomosynthesis (commonly known as three-dimensional [3D] mammography).
Many studies have found that 3D mammography appears to lower the chance of being called back for follow-up testing. It can also be more helpful than a 2D mammogram to evaluate dense breasts (more common in younger women).
Ultrasound is also better at evaluating dense breast tissue. People under 30 have more dense breasts.
UNDERSTANDING MAMMOGRAM RESULTS:
“Dense Breasts” are more common in younger women. As we get older, we have more fat versus glands and ducts. If over 75% of breast tissue is glands and ducts, you have “dense breasts.” Dense breasts make iit harder to find cancers on mammograms because the glands, ducts, and cancers all show up looking white on the images.
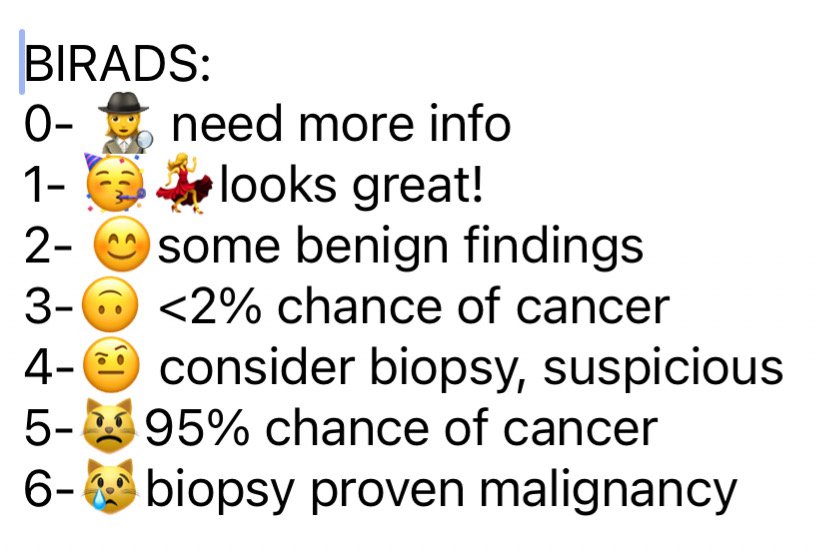
BIRADS SCALE:
Each mammogram will have a BIRADS scale number assigned to it, which tells you how likely the results are to be cancer. Using emojis, here are what the different BIRADS categories mean:
Save this image to help you better understand your mammogram results! The meaning of BIRADS on your mammogram.
SHOULD YOU BE WORRIED ABOUT RADIATION FROM MAMMOGRAMS?
A mammogram is one of the lowest levels of diagnostic radiation. One mammogram is equal to the radiation exposure you accumulate from existing for 3 months on earth.
I asked a radiologist at my work about any radiation concerns and he said, "Getting a mammogram should not even be a question about radiation concerns,” -Dr Nick Costouros.
Our bodies have mechanisms to deal to with low levels of radiation. Otherwise our cells would be becoming malignant everyday. We have daily exposures from living in a house (radon), driving a car, walking outside (the sun) and even more so when getting on a plane! Cosmic rays cause radiation that is normally fractured by our atmosphere, so when we fly, we are exposed to more radiation. We take risks every single day, but we are comfortable to those risks and don't even question them.
When providers are ordering diagnostic imaging, they are always considering cost/risk versus benefit analysis. If they have placed an order for you, they have deemed that the benefit from knowing the test result is greater than any risks associated with performing the test (same goes for ordering a medication or any treatment).
MRI has NO radiation- it’s magnets and radio waves (recommended for HIGH risk of developing breast cancer).
ALL of these kinds of diagnostic imaging provides radiation below the threshold that we can measure cause and effect.
WAIT… WHAT?!? NO SELF BREAST EXAMS?
The recommendation was made after data review concluded there was not strong evidence to support monthly exams for women at average risk. Masses felt during breast exams are more likely to be benign and can lead to an increase in anxiety and unnecessary testing. They can also provide a false sense of assurance and should never be a reason to delay screening imaging.
Almost all providers and guidelines agree: Breast Awareness > Monthly Self Exams. Get to know your breasts, what they normally look and feel like and report any changes LIKE: new lumps, bumps, swelling, pain or skin changes right away to your doctor. Note that pain is only a symptoms of cancer for 5% of breast cancer diagnoses.
Most people are surprised to hear that ‘Research has not shown a clear benefit of regular physical breast exams.’ Photo by Laura Pope Photography.
“Research has not shown a clear benefit of regular physical breast exams done by either a health professional (clinical breast exams) or by women themselves (breast self-exams). There is very little evidence that these tests help find breast cancer early when women also get screening mammograms. Most often when breast cancer is detected because of symptoms (such as a lump), a woman discovers the symptom during usual activities such as bathing or dressing. Women should be familiar with how their breasts normally look and feel and should report any changes to a health care provider right away. But it’s important to understand that there is very little evidence that doing these exams routinely is helpful for women at average risk of breast cancer)” American Cancer Society Recommendations for Early Detection of Breast Cancer.
I tested positive for a genetic cancer-causing mutation. Photo by Laura Pope Photography.
TESTING POSITIVE FOR A CANCER-CAUSING GENE MUTATION
I got a call with the results as I was recovering at home from my C-section with my newborn baby in my arms: I tested positive (not good) for a cancer-causing gene mutation in my DNA. I immediately thought “was it a mistake having kids and passing down my ‘faulty’ genetic material that can cause disease?”
After realizing that (a) while pregnant is NOT the best time to have genetic testing done and (b) we all can have imperfect genetic codes that we are born with, and many people NEVER know about them. This information is GOOD and is simply that: more information. I knew before testing that it was likely I could have a gene mutation, as I had a family member test positive. Originally, Kaiser only wanted to test me for that specific gene, but I advocated for a full genetic panel, as there were a few people with cancer on my other parent’s side (we inherit genes from both mom and dad).
I had decided I would want to know, as it could help to justify earlier screenings for cancer. Early/regular screenings means a higher likelihood of being able to watch my kids grow, learn to drive, and walk down the aisle. It would increase my chances of experiencing the privilege of growing old with my husband.
Positive Genetic Results provided the justification to begin screening early at 35 with mammograms
MY FIRST MAMMOGRAM
The positive genetic results gave the justification for Kaiser to approve for me to have my first screening mammogram with tomosynthesis at 35 years old. It was surprisingly NOT painful and a lot less drama than I was expecting. In fact, I quite liked having some quiet time to myself with two small kids at home! I feel better knowing I am doing something to help reduce my risk and control what I can with my health (exercising, eating more veggies and cutting back on champagne is a continued work in progress;)