What Your Postpartum Nurse Wants You to Know
I’d love to connect with you on Instagram, where I share home, health and lifestyle tips!
I have quite literally assembled my “A” team to bring you everyone’s best tips! Thank you to all of the amazing Postpartum nurses, moms, and women I spoke to for this community-post. I hope you find something useful here, no matter what type of birth you have.
For many women, the day their baby is born is one of the best days of their lives. Some women also consider birth a traumatic experience. One thing is for sure: you are a different person than the one before birth, and that is a GOOD thing.
Little Nuggets of Motherly Wisdom: Trust your Gut. There is no one better to care for your baby than YOU. Be kind to yourself. Ask for help. Fancy Snacks (breastfeeding is a lot of work!).
THE HOSPITAL EXPERIENCE:
You can typically expect to be at the hospital for up to 3-4 nights if you had a C-Section. If you delivered vaginally, insurance will pay for 48 hours, but it’s OK to leave 24 hours after the baby was born.
Wow!!! You just had a baby exit your body! What’s next?
When you arrive in the Mother-Baby Unit, each of the nurses will check your bleeding (lochia), MASSAGE YOUR UTERUS, and check your incision if you had a C-Section. The uterus massage sounds nice, but it really is not. They do this to help your uterus contract and stop bleeding. IT CAN BE PAINFUL. Another time your uterus will contract (and it can be painful)? While you are breastfeeding!
THE “SECRET MENU” ON THE POSTPARTUM UNIT
The following are items you can talk to your nurse about to decide if they might be helpful:
THE NURSERY: The reason the nursery is hush-hush and a bit controversial is that it is part of an initiative to get more moms to breastfeed (Do Baby Friendly Hospitals Work for All Moms? Article). Not every hospital offers this, but you can talk to your nurse to see if the nursery is something available and you can decide if it might be helpful for you.
NARCOTICS: Some women don’t need them, so they are given only “as needed” (or when you ask for them). They are typically available every 4-6 hours. If you have pain over a 5 or 6/10, you can talk to your nurse about narcotic pain medication. I could really do a post or two on the opioid epidemic, but as long as you are taking pain medicine when you have pain, then you are not addicted. Be sure to continue to stay on schedule with tylenol and motrin (those should be scheduled), walk to prevent gas pain if you had a C-Section, and use the tips in the video below for natural pain management.
LANOLIN: “We don’t automatically give out because a lot of people have their own and colostrum rubbed into the nipples is more effective.”
My friend from high school, Bri Dietz, is three kids deep and made a little video about her postpartum experience with some of her best tips. I LOVE her candor and I think you will really appreciate her advice!! You can connect with Bri on Instagram for more of her, her adorable kids and experience of motherhood in San Diego.
Click on the photo (or here) to watch mama of 3, Bri Dietz, share the real and the raw of postpartum!
POSTPARTUM NATURAL PAIN MANAGEMENT:
The video below highlights the “bathroom situation” and natural pain management tips for both vaginal and C-section births.
You should also try to pee every 2 hours, especially before breastfeeding, which can help with cramping pain.
Walking: If you had a C-Section, try to get up and walk as soon as possible. Walking will help to prevent blood clots, help you have a bowel movement, with healing, and will help to prevent gas pains (which can be very uncomfortable).
GO SLOW AND LISTEN TO YOUR BODY. If you have stitches from tearing or had a C-Section, be really careful about going too hard after birth, particularly once you’re home. You have to be really conscientious about taking it easy.
Post vaginal delivery AKA “POSTPARTUM PERINEAL PAMPERING”: Your uterus has a dinner-plate sized wound where the placenta was attached. Expect a LOT of bleeding and some blood clots, especially for the first 10 days. It tapers off (into yellow/white lochia) over then next 6 weeks. NO TAMPONS!! You can get an infection if you use tampons. Some women love to use the Always Adult Diapers instead of (or in addition to) pads.
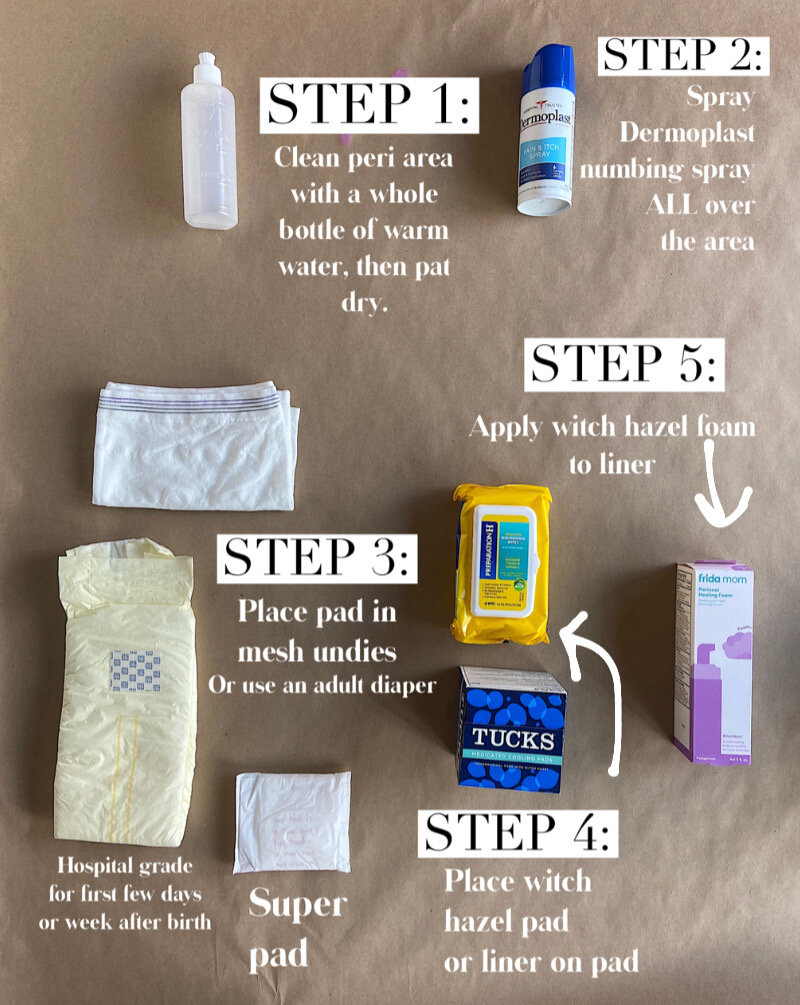
COLD PACK HACK: Use a newborn diaper, peel open the back and fill with ice. Place 2 witch hazel “wipes” (I found Preparation H wipes at Costco and they were so cheap! You could alternately use Tucks). On top of the witch hazel wipe, place 4-5 pumps of witch hazel foam on top (the only brand I found was FridaMom Perineal Healing Foam). It’s also a good idea to have some Preparation H cream around for hemorrhoids that can develop during delivery.
If you don’t want to deal with the diaper ice, these ice packs have washable soft covers and great reviews!
I have heard some rave reviews about this Frida Mom upside-down Peri Bottle. If you have stitches, it can be really helpful! Be sure to use WARM water.
After a C-Section: Use a regular pad and mesh panty OR adult diaper. You only need really thick pads the first day or few, then most women have some light bleeding for 2 weeks or so. No tampons!
You will have a dressing over your incision that usually comes off after 24 hours, then it’s OK to shower. Under the dressing will be steri-strips that fall off after 7-10 days. You may have glue under the steri-strips, keeping the incision together. Place an ice pack over your incision, then your hospital-issued abdominal binder. If you are tall, ask for a tall binder and be sure to stash one or two in your bag to bring home! Place the K-Pad (heating pad in the hospital, ask your nurse for it) or electrical heating pad from home on the upper part of your belly to help with cramping. You may also have pain in your shoulder or abdomen, and the heat helps with that too (as does walking). Simethicone can be really helpful for gas pain as well.
You may want to switch to a more deluxe abdominal binder (like one of these) or C-Section undies for more support.
THE FIRST TIME YOU PEE AFTER BIRTH:
Put some mint aromatherapy oil in the toilet and it will help you pee (I have no idea how this works), compliments of the Vagina Whisperer! Try to relax and run the faucet water. Again, trying to pee every 2 hours will help with cramping.
THE FIRST TIME YOU POOP AFTER BIRTH:
This can be uncomfortable, but it’s important not to strain, particularly if you have stitches. Drink plenty of water during your stay. You may be started on colace or colace and senna (stool softener and very mild laxative) after birth to prevent and treat firm stools and constipation if you had a C-Section. Continue to take these at home, particularly if you are taking narcotics.
Click here for a guide to over-the-counter remedies for constipation, as well as an all-natural remedy for constipation that you can make while you’re pregnant and keep in the fridge.
BREASTFEEDING:
TakingCaraBabies is an awesome resource for all things babies and kids. HERE IS AN AMAZING VIDEO OF HER SHOWING YOU HOW TO BREASTFEED WITH A SUBWAY SANDWICH. I also highly recommend checking out her resources for getting babies to sleep and stay asleep (she has a whole program!).
Breastfeeding is (quite literally) magical. Karen Lisbon, RN, BSN, IBCLC explains, “When a mother smells or kisses her baby, her ‘milk making ‘factory"‘ receives information and produces antibodies to strengthen baby’s immune system through the lymphatic system.”
A lot of women expect breastfeeding to be this innate, natural process, but the truth is that for most women it takes WORK. In our society, women don’t have very many opportunities to watch breastfeeding up-close before it’s their turn to learn. You and your baby have to learn something new together and it can take some time. Ask for help.
Your nipples have to “toughen up” initially, which can be really tender and it takes a few weeks. Stick with it! Make sure your provider (doula, midwife, nurse) watches your baby feed and ask them for pointers. If feeding is painful or you are a first-timer, ask for a lactation consult so you can learn more about getting a deeper latch before you go home. If you are home already, ask your OB or baby’s pediatrician for a referral. KellyMom is an amazing resource for all things breastfeeding and if it is painful for you, this post is helpful. Pain/tenderness is normal, particularly right when the baby latches on. If it doesn’t resolve, make sure baby’s chin is pulled down and lips are rolled out. If that doesn’t help, gently insert a finger to help softly break the latch and start again. “If you’re experiencing pain that makes you dread feeding your baby or that you describe as excruciating or if you have cracked or bleeding nipples, then this is NOT typical and there is almost always something that can be done to address the issue and to alleviate the pain.” (KellyMom).
For scabbed or raw nipples: use a baby wipe or wet paper towel to wipe nipples clean after feeding to wipe away baby saliva. Squeeze out a little colostrum or milk and massage into nipple. Then place CHILLED Medela Soothing Gel Pad over each nipple. You can reuse each pad for 24 hours. Enjoy that sweet relief!
Whichever delivery route, milk usually ‘comes in’ about 2-6 days after birth. Before your milk ‘comes in,’ you produce colostrum or “liquid gold.” If your milk is slow to come in, try not to worry. Babis can do really well on colostrum alone in the early days (Kellymom). Practice lots of skin to skin contact and see below for information on how to tell if your baby is getting enough from your colostrum or breastmilk, under “Your Baby.”
Breastmilk is supply and demand. You can hand express or pump to create or increase the demand.
This is a little controversial, but if you are concerned about milk supply, ask your doctor if it would be safe for you to start hand-expressing at 32 weeks. You can also talk to your doctor about taking Fenugreek supplements after birth. Fenugreek is the actual ingredient in all of the lactation teas and cookies, but these are the doses you actually need to help with milk production. Here is more info on supplementing from Kaiser with Fenugreek, then talk to your doctor if it’s right for you (it can cause low blood sugars and GI issues in both baby and mom). Putting the baby on the breast and plenty of skin to skin helps with milk production.
“The American College of Obstetricians and Gynecologists recommends mothers exclusively breastfeed their babies for the first six months of life, but ACOG also officially recognizes that a baby's mother "is uniquely qualified to decide whether exclusive breastfeeding, mixed feeding or formula feeding is optimal for her and her infant” (Motherly). Be sure to talk to your baby’s pediatrician about any feeding concerns.
Rule number one: Feed the baby. Don’t freak out if the pediatrician recommends supplementing with formula, and it may very well be temporary. What your baby needs is enough calories and a mom who can be present. If you feel that any aspect of motherhood is causing you psychological stress, speak to your physician about it.
"I always support the idea to breastfeed if you can, to reach out for support, and if you are struggling, there are other safe and healthy options to ensure your baby is well fed," (Dr Liu, to Motherly).
However you decide to feed your baby, you are a great mom and I support you. Thank you for Felicia Saunders Photography for this beautiful image showing there are many ways to nourish a baby.
YOUR BABY:
Your baby may be QUITE sleepy, or they may not be and either is OK. One weird thing that can happen is babies can develop lumps under their nipples and breastmilk will actually come out if you press! This is actually normal and just their response to mom’s hormones. Their first poops are cray-zay!! They are called “meconium” and are a dark, dark forrest green. Don’t be alarmed.
How to know baby is getting enough milk from birth to 6 weeks (from KellyMom.com, amazing breastfeeding and pumping resource!):
WEIGHT GAIN:
”If baby is gaining well on mom’s milk alone, then baby is getting enough. A 5-7% weight loss during the first 3-4 days after birth is normal. Baby should regain birth weight by 10-14 days. By day 5, average weight gain is 2/3-1 oz per day (5-7 oz/week). If these goals are not met, call your lactation consultant (or ask for a referral from your pediatrician).
WET DIAPERS: 6+ wet diapers per day (by day 4).
Expect one wet diaper on day one, increasing to 6+ by day 4. To feel what a sufficiently wet diaper is like, pour 3 tablespoons (45 mL) of water into a clean diaper (if baby wets more often, then the amount of urine per diaper may be less). Urine should be pale and mild smelling.
DIRTY DIAPERS: 3 – 4+ dirty diapers per day (by day 4).
Stools should be yellow (no meconium) by day 5 and the size of a US quarter (2.5 cm) or larger. The normal stool of a breastfed baby is usually yellow and is loose (soft to watery, may be seedy or curdy).
OTHER POSITIVE SIGNS: After a feeding, mom’s breast feels softer and baby seems reasonably content. Baby is alert, active and meeting developmental milestones.” (KellyMom).
It takes some time (months) for your uterus to shrink back to it’s normal size. Give it time!!
YOUR BODY
It takes some time for your uterus to shrink back down to it’s regular size (when your uterus contracts during BF, that’s what it’s working on). Ali Wong described breastfeeding as, “this savage ritual that just reminds you that your body is a cafeteria now! It don't belong to you no more." Give yourself GRACE. There will be a time your body doesn’t feel like your own, and that’s OK. It’s a season. The days are long but the months are short and before you know it, you won’t be breastfeeding anymore (and you will have a toddler who is running around, throwing all kinds of things in the toilet!).
I think there should be a fine anytime someone mentions “Getting your body back.” It’s good to return to exercise slowly for your physical and mental health, but there are a bajillion more important things than ‘getting your body back.’
Some women sweat profusely during the night after birth and others don’t (I never did).
Try to find other ways to connect with your partner while you are on pelvic rest (for 6-8 weeks until healed).
There are a variety of issues (and some unpleasant surprises) you can run into after birth. Talk to your doctor about any concerns you have and for most issues, a referral to a pelvic floor physical therapist can work wonders!
Diastasis Recti is when the abdominal muscles separate. (click on the link for a video on how to check yourself postpartum if you are worried). There are exercises you can do to help!
After pelvic rest, Sex can be painful due to dryness from breastfeeding and tight muscles. Lube can help, as well as perineal massage and a referral to a pelvic PT. Check out info from The Vagina Whisperer here on Postpartum Sex.
Urinary incontinence is common, but not normal. Ask for a referral to a pelvic floor PT for help.
Your first postpartum period is going to be a situation. The Vagina Whisperer also has some advice for you about Post-Partum Periods.
D-MER is a transient negative or devastating emotions during milk letdown.
MEALS:
Meal Train, Meal Train and Meal Train. I was SO hesitant about allowing my friend to set up a Meal Train for us because I REALLY did not want to have to make small talk with a bunch of people I didn’t know well. I even arranged initially to have them leave the food in a cooler on our porch. In the end, it was the BEST experience and I only wish we had set up more dates! Some of the best food I’ve ever had was made by friends. Everyone was really respectful and when we invited them in, they only stayed for a few minutes (sometimes it felt like they were running away and we were like, “no, stay!!!”). We felt less lonely and really taken-care-of by our community. DO IT!!!
If a Meal Train is not an option, you can stock up on food by preparing Crock Pot recipes ahead of time and Costco has tons of great meal options that are ready-made.
YOUR MIND:
There are SO MANY physical changes that happen after pregnancy and childbirth, but they only represent a portion of how you change when becoming a mother. Society (and let’s face it, some of our families!) can be really hard on moms and it can feel like the whole world is judging you. You may also feel really disappointed or even traumatized about how the birth went or how motherhood or breastfeeding are going. For all the progress we have made as moms, the actual changes and challenges involved in becoming a mom are rarely spoken about. In order to take care of yourself (and therefore your baby), ASK FOR THE HELP YOU NEED.
WE WERE NEVER MEANT TO DO THIS ALONE.
I was shy about asking for specific help with my son’ birth. This time, I’m going to be more direct by asking family to help with dishes, or to hold the baby so we can nap, etc. People want to help, but they need some direction, so speak up!
POSTPARTUM DEPRESSION:
It would be helpful to look over this list and have your partner or support person look over this list. If you notice any of these feelings that are persisting for over a week or so, talk to your doctor right away.
Feeling sad, hopeless, empty, or overwhelmed
Crying more often than usual or for no apparent reason
Worrying or feeling overly anxious
Feeling moody, irritable, or restless
Oversleeping, or being unable to sleep even when her baby is asleep
Having trouble concentrating, remembering details, and making decisions
Experiencing anger or rage
Losing interest in activities that are usually enjoyable
Suffering from physical aches and pains, including frequent headaches, stomach problems, and muscle pain
Eating too little or too much
Withdrawing from or avoiding friends and family
Having trouble bonding or forming an emotional attachment with her baby
Persistently doubting her ability to care for her baby
Thinking about harming herself or her baby (talk to your provider right away)
“The “baby blues” is a term used to describe the feelings of worry, unhappiness, and fatigue that many women experience after having a baby. Babies require a lot of care, so it’s normal for mothers to be worried about, or tired from, providing that care. Baby blues, which affects up to 80 percent of mothers, includes feelings that are somewhat mild, last a week or two, and go away on their own.
With postpartum depression, feelings of sadness and anxiety can be extreme and might interfere with a woman’s ability to care for herself or her family. Because of the severity of the symptoms, postpartum depression usually requires treatment. The condition, which occurs in nearly 15 percent of births, may begin shortly before or any time after childbirth, but commonly begins between a week and a month after delivery” (National Institute of Mental Health).
“Estimates of the prevalence of paternal postpartum depression (PPD) in the first two months postpartum vary in the postpartum period from 4 to 25 percent” (Sad Dads). If the baby’s father is experiencing psychological stress, he should speak to his physician and ask for help.
MORE RESOURCES:
Other Helpful Posts for New Parents: Baby Registry Must Haves, How to Survive the Newborn Phase, and How to Help a Choking Baby.
I found these articles really helpful. Click on an article below to learn more:
How To Overcome- And Heal From- A Traumatic Birth
The Pressure to Exclusively Breastfeed is hurting Mothers’ Mental Health
Here are some great resources for Postpartum Depression and Anxiety.
To learn more PTSD and trauma after childbirth, click here (SolaceforMothers.org).
TakingCaraBabies is an amazing resource for all things baby
The Vagina Whisperer Post Partum physical therapist and your vagina’s new BFF