What Your Labor And Delivery Nurse Didn't Tell You
I’d love to connect with you on Instagram, where I share home, health and lifestyle tips!
Other Helpful Posts for New Moms: What your Postpartum Nurse Wants you to Know, Baby Registry Must Haves, How to Survive the Newborn Phase, and How to Help a Choking Baby.
When I get nervous about birth, I like to remind myself that our bodies were quite literally designed to give birth and women have been doing it for thousands of years. It’s kind of like a hazing into motherhood, but I don’t seem to hear much about the actual labor/birth process, even amongst moms.
Every mama has a unique birth experience, but there are some basic ways to prepare for birth. You may be the personality type to want to take a class/course/read all the books or you may only want the down and dirty basics. For some birth basics, I liked this article I found from Today’s Parent that has some tips for preparing you and your partner for Labor and Birth. It also has a great, short video at the end going over the stages of labor.
Part of having a positive birth experience is preparing to be flexible and surrounding yourself with good support. Your nurse is with you the majority of your labor and the doctor usually comes in after you have started to push. You will be randomly assigned a nurse for one of life’s biggest moments.
One thing nurses don’t mention? You can ask for a different nurse (Doctors too!).
Yes, it’s a little bit drastic, but particularly if you don’t feel safe or comfortable, let them know you would like a different nurse. If you are confrontation avoidant, you can press your call-light (button) and ask to talk to the charge nurse. When she comes in, explain that you would like a new nurse. You have the right to feel safe and comfortable for your birth experience!
Are you planning on having a C-Section? If so, head on over here for all the C-Section tips!
I have been peppering birth professionals for months to get the real scoop that isn’t covered in any online article or book. I spoke to an anesthesiologist, OBGYN, and over 15 Labor and Delivery (L+D) nurses (some of which have been on that unit for 20+ years!).
What your Labor and Delivery Nurse Didn’t tell you
Here are their cumulative answers:
Ok… how many people poop during delivery and do you ACTUALLY “not mind” if it happens?
L+D RNs: About half of women poop during delivery. It’s not usually an entire bowel movement, but more or less little bits at a time while you push since you use the exact same muscles to push baby out as you do to have a bowel movement. Nurses expect it. We don’t care. It truly is nothing to be concerned about and we just fold up the pad underneath you and replace it with a new one. No big deal. Also, almost 90% of women shake violently and vomit during labor. It’s completely normal and due to the hormones.
What are your opinions on Birth Plans?
L+D RNs: It’s a good idea to research all of the options and be educated about what different interventions the team may offer (see the end of this post for a list). Most importantly, BE FLEXIBLE! Everything can change so quickly. One nurse said, “The most important thing to remember is everyone’s goal is to deliver a safe, healthy baby to a safe, healthy mom.“ Another said, “Epidurals are the best thing ever invented. One of my patients said giving birth felt like a 25 pound weight pulling her insides out, then after she had an epidural she was resting quietly.” Another RN commented that “you want to enjoy that moment (of giving birth), you don’t want to forget because the pain was so intense.” Some women may want to forgo any interventions for pain, and that is completely their decision. Do you want to try a different position? Speak up and ask your partner to do the same! You can ask if you can take a shower, use the peanut ball, change positions, etc.
Do epidurals really slow down the labor process?
Anesthesiologist: Epidurals VERY rarely slow down labor progression. This only happens if a woman wasn’t actually in productive labor (consistent contractions about every 3 minutes with some cervical dilation) when it was placed. The only “risk” to getting an epidural “too early” is that you can’t get up and walk, you need a Foley catheter, and cannot eat (to prevent aspiration if an emergency c-section was needed). They have to give a test dose once the epidural is placed, so once the catheter is in, you can’t walk around. The goal of an epidural is to manage pain so that moms can focus/concentrate, but not be so numb that they cannot feel contractions.
What is a ‘Walking Epidural’?
Note: Not all hospitals offer Walking Epidurals. Anesthesiologist: An epidural contains 2 medications: Fentanyl and bupivicaine. Fentanyl can be given alone, also known as a “walking epidural.” You can still walk and feel contractions but the spinal epidural with bupivicaine is what numbs contractions (and your legs). Fentanyl given through an epidural is more effective than IV fentanyl. IV fentanyl causes some drowsiness, where Fentanyl given through an epidural does not. They do not give IV fentanyl if baby is expected to come out within 2 hours.
When should you ask for an epidural?
Anesthesiologist: You should let the team know when you arrive if your plan is to have an epidural. Some moms say they want to “wait and see.” You should ask for an epidural when your pain is 2 less than pain that you cannot tolerate. For example, if 6/10 pain is too uncomfortable for you, then when your contractions are 4/10, you should ask for the epidural. You need to be able to sit still for 10-15 minutes, curled over to have the epidural placed, which is extremely difficult if you are already in too much pain.
Technically we don’t like to place epidurals while a patient is transitioning (meaning once they are dilated between 7-10cm). The epidural will not be completely effective if it is placed too late, as ‘multips,’ or second time moms, may “transition” quickly and only push for 15 minutes after they are fully dilated.
I saw a nurse on Instagram mention that she would “do everything she could” to NOT get antibiotics if she was Group B Strep Positive (GBS). What do you think about that?
L+D RNs: That is incredibly dangerous. Doctors test patients by doing a perineal swab between 36-37 weeks of pregnancy and 1 in 4 moms test positive. It can come and go (meaning if you tested positive for your first baby, you might be negative for the second). The bacteria lives in your perineum and can be spread to the baby during labor (which is why antibiotics are given during labor). There is about a 5% chance of a baby dying from GBS infection if they contract the infection. The babies get really sick really fast and it can also cause brain damage/mental handicaps.
All the tips to have a successful Labor and Delivery
What would you tell a patient who was considering a home birth?
OBGYN: I would find out more about why they would be interested in a home birth. Are they nervous that they will have medical interventions ‘pushed’ upon them? Are they afraid of hospitals? Then I would want to work together with them to figure out how we can meet their needs while still providing access to quick emergency care.
What are your opinions on Doulas?
L+D RNs: The birth room should be calming, feel comfortable and be mama-centered. A good doula can be invaluable to help you find techniques to focus during pushing. You certainly do not have to have a doula. You could alternatively make sure you have a support person who can help you focus. Some women like to bring a picture or object to focus on. If a doula is adversarial to the care team and focuses too much on rigidity, they can make the environment toxic, but the vast majority are very helpful to have.
What you ACTUALLY need to bring to hospital:
If you are expecting to deliver the baby vaginally, you can expect to be at the hospital for 1-2 nights. If you have a C-Section, it is usually a 3-4 night stay.
The hospital has everything you NEED to ‘survive’ your stay (besides phone chargers and you need a car seat to go home), so just remember that as you are packing up half of your car! You are basically packing ‘Creature Comforts’.
Also remember: the hospital is DIRTY, DIRTY, DIRTY. Anything you bring to the hospital (clothing-wise) should be washed when you get home and slippers should be washed or cleaned well. These are all jobs and you won’t feel much like doing jobs when you get home, so less is more!
“Bring Your Own Toiletries” when you are packing your hospital bag for birth.
TRACI’S TIP: I have a toiletries travel case loaded in my closet that is always ready-to-travel. I restock the products when I come home from a trip, so it’s a breeze when it’s time to pack. I also try to include really lovely/fancy travel size products as an extra luxury!
The “Essentials”:
CAR SEAT: most hospitals will require you to load baby into it in your room. 4 out of 5 car seats are improperly installed, so make sure yours is done correctly by going to a Carseat Installment Check. (Google Search: “Car Seat Installment Check + Your City”). CHP also checks installment for free, requires an appointment (Find your local CHP here, then call to make an appointment).
CELL PHONE CHARGER
ONE BABY OUTFIT to bring baby home in (should be pants so they can be strapped into car seat)
ONE MAMA OUTFIT to go home in
FLIP FLOPS for shower and walking around the unit (you could use slippers instead, but then you don’t have for the shower)
SOFT NURSING BRA so you don’t jiggle-jaggle
Soft and Cozy SOCKS
Your favorite TOOTHBRUSH AND TOOTHPASTE
DEODORANT
LIP BALM
SNACKS and Drinks for Dad!!
HAIR TIE+ if you have bangs. bring a headband
MAKEUP REMOVER WIPES
PACIFIER (this is a bit controversial, as it can create ‘nipple confusion,’ but we used one)
Download GUVA WHITE NOISE APP on your phone for white noise for baby
MEDELA SOOTHING GEL PADS: these are a MUST if you breastfeed. Sweet relief!
Your insurance is required to provide you with a breast pump after delivery. I bought the Spectra instead, and it’s a great idea to have it in the car (along with a hands-free pumping bra), in case you need to pump in the hospital. If you want to use the pump provided by your insurance (call the number on the back of your insurance card when you are pregnant to get the scoop), then just bring the HANDS FREE PUMP BRA, in case.
Optional Add-Ons:NICE PILLOWS for you and your partner. Pack this in a large BAGGU nylon foldable bag.
ELECTRIC CANDLE (some nurses would make you leave a light on if you don’t have this)
BUCKY EYE MASK (the room is not very dark and your partner will especially need. An ER nurse shared this particular mask with me 10 years ago and I have since been obsessed)
FANCY SOAP (the shower after birth/C-Section is the most amazing shower of your life, take advantage!)
GUM (if you are told to stop eating, you still may be able to chew gum and it may help with nausea)
HAIR NEEDS like dry shampoo or travel Shampoo/Conditioner
MAKEUP (there are so many photos taken I chose to bring and use a little. It also made me feel more human)
Your own, soft PAJAMAS OR NIGHTGOWN (make sure it buttons up or has easy boobie access)
ROBE for walking around the halls (although the hospital usually provides an extra hospital gown)
NURSING PILLOW (make sure you have an extra, clean cover for home). I used the BBHUGME because the My Breast Friend is a little hard to use in bed. I also used this to support grandma and other kids while holding the baby ay home (note, most hospitals ONLY allow direct siblings to visit)
BABY ACCESSORIES FOR PHOTOS: like an extra outfit or two, headbands or swaddles if you care or plan to take photos
A way to PLAY MUSIC OR WATCH SHOWS (or you can ask at hospital tour about their set-up)
I always travel with a few extra BAGGU foldable nylon bags for laundry, dirty shoes, and you can use for hospital supplies, etc.
BABY MONITORS
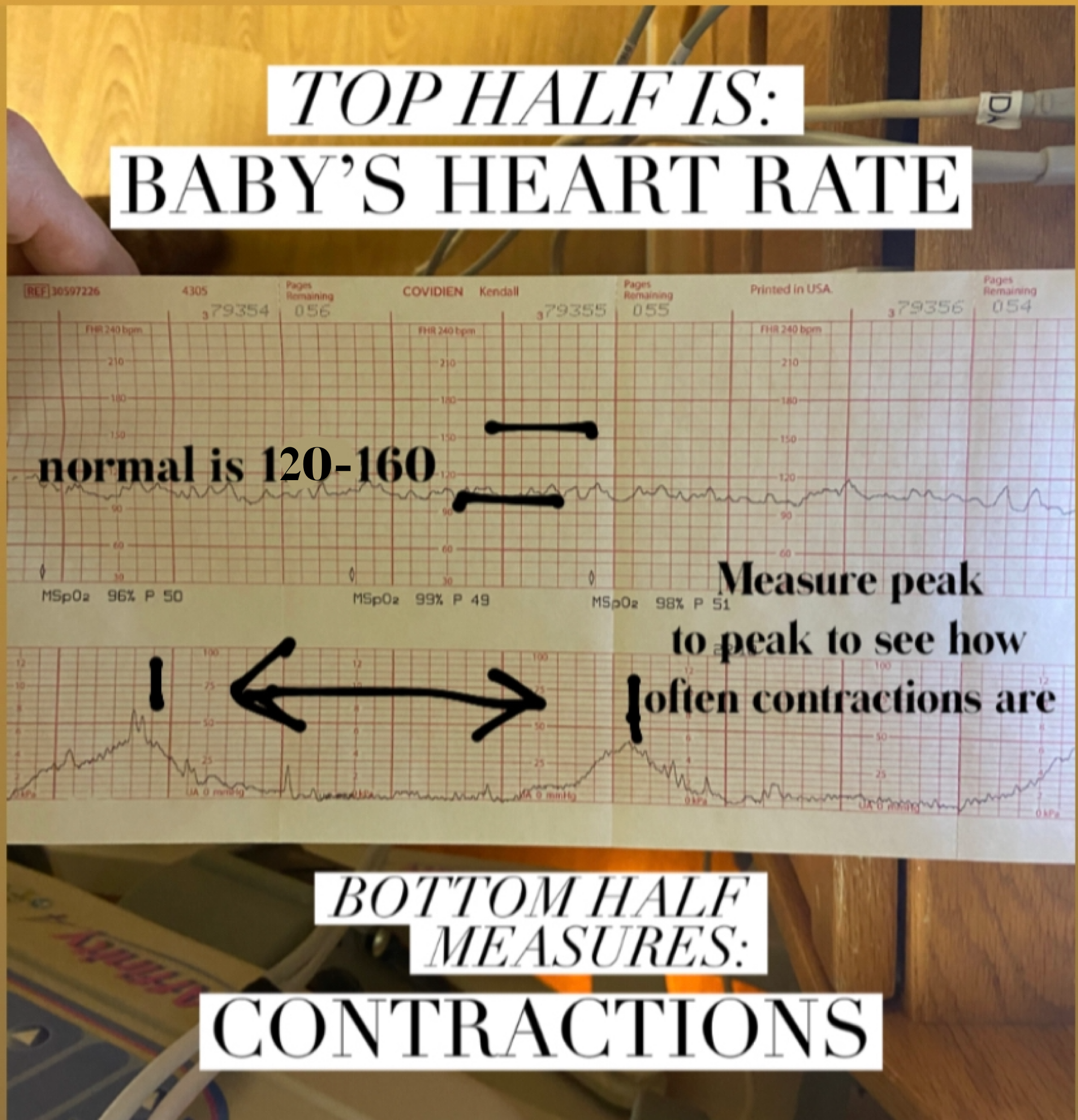
What are you looking for with the monitors?
The nurses will be using the monitors as part of their assessment and you never need to look at them or know what they mean. In fact, I would recommend that you not try to watch the monitors and focus on how you feel (or how your partner is feeling if you are a support person). Your nurse and the physicians are watching these monitors in your room, at the nurse’s station, and possibly even on their phones!. One of the monitors is tracking the frequency and length of contractions (TOCO monitor) and the other monitors baby’s heart rate in relation to the uterine contractions. When you get up to go to the bathroom, you can unplug quickly, but if you are going for a walk, you need to wear a small portable monitor. They are looking to make sure baby’s heart beat is within a normal range and is responding well to contractions. They are also looking to see how long and regular your contractions are (the monitor is not 1:1 with contraction pressure though, they tell that be feeling your belly). Note: This is a simplified explanation and there is a lot more knowledge and experience involved to actually interpret fetal monitoring.
How the nurses read the fetal heart and TOCO uterine contraction monitors during Labor and Delivery.
Different Interventions that are offered during delivery:
Pain Relief: IV nubain, nitrous oxide (laughing gas), walking, positional changes, cold/heat, tub, epidural
To help create organized and strong contractions: Pitocin (oxytocin) is given IV. This is the same hormone that your body makes after delivery and during breastfeeding that causes uterine contractions. The dose is progressively escalated to increase frequency and strength of contractions.
If the tracings/monitor isn’t great: IV fluids, position change (flip to your left side as baby can push on your largest heart blood vessel while laying flat on back),
Induction: Cytotec (misoprostyl) or Cervidil to soften and thin cervix. FUN FACT: the main ingredient in these cervix ‘ripeners’ is prostaglandin, which is found in sperm. This is why it’s recommended to have sex to induce labor! Foley Bulb or Cooks Catheter: a small balloon blown up inside the the cervix with saline inside at 1-2 cm to mechanically stretch the cervix to 4-5cm.